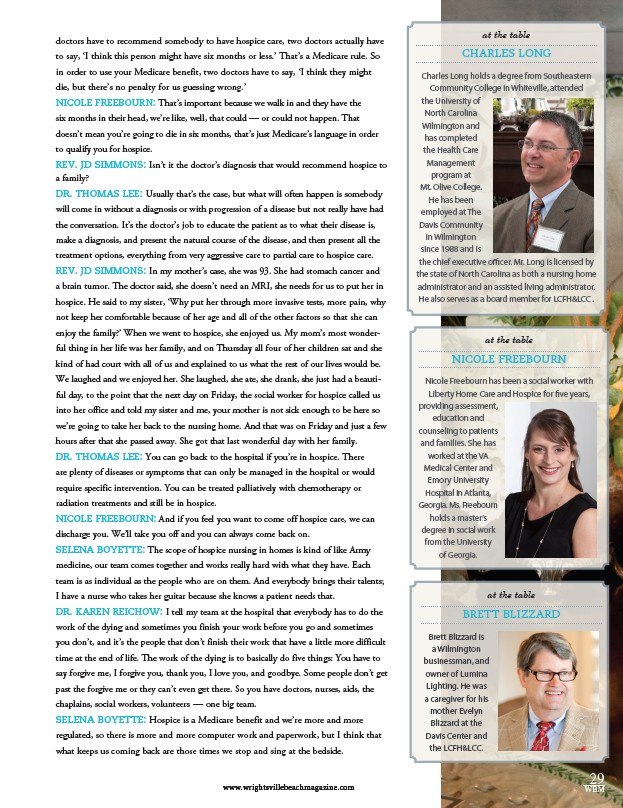
Charles Long holds a degree from Southeastern
Community College in Whiteville, attended
the University of
North Carolina
Wilmington and
has completed
the Health Care
Management
program at
Mt. Olive College.
He has been
employed at The
Davis Community
in Wilmington
since 1988 and is
the chief executive officer. Mr. Long is licensed by
the state of North Carolina as both a nursing home
administrator and an assisted living administrator.
He also serves as a board member for LCFH&LCC .
Nicole Freebourn has been a social worker with
Liberty Home Care and Hospice for five years,
providing assessment,
29
at the table
CHARLES LONG
doctors have to recommend somebody to have hospice care, two doctors actually have
to say, ‘I think this person might have six months or less.’ That’s a Medicare rule. So
in order to use your Medicare benefit, two doctors have to say, ‘I think they might
die, but there’s no penalty for us guessing wrong.’
NICOLE FREEBOURN: That’s important because we walk in and they have the
six months in their head, we’re like, well, that could — or could not happen. That
doesn’t mean you’re going to die in six months, that’s just Medicare’s language in order
to qualify you for hospice.
REV. JD SIMMONS: Isn’t it the doctor’s diagnosis that would recommend hospice to
a family?
DR. THOMAS LEE: Usually that’s the case, but what will often happen is somebody
will come in without a diagnosis or with progression of a disease but not really have had
the conversation. It’s the doctor’s job to educate the patient as to what their disease is,
make a diagnosis, and present the natural course of the disease, and then present all the
treatment options, everything from very aggressive care to partial care to hospice care.
REV. JD SIMMONS: In my mother’s case, she was 93. She had stomach cancer and
a brain tumor. The doctor said, she doesn’t need an MRI, she needs for us to put her in
hospice. He said to my sister, ‘Why put her through more invasive tests, more pain, why
not keep her comfortable because of her age and all of the other factors so that she can
enjoy the family?’ When we went to hospice, she enjoyed us. My mom’s most wonder-ful
thing in her life was her family, and on Thursday all four of her children sat and she
kind of had court with all of us and explained to us what the rest of our lives would be.
We laughed and we enjoyed her. She laughed, she ate, she drank, she just had a beauti-ful
day, to the point that the next day on Friday, the social worker for hospice called us
into her office and told my sister and me, your mother is not sick enough to be here so
we’re going to take her back to the nursing home. And that was on Friday and just a few
hours after that she passed away. She got that last wonderful day with her family.
DR. THOMAS LEE: You can go back to the hospital if you’re in hospice. There
are plenty of diseases or symptoms that can only be managed in the hospital or would
require specific intervention. You can be treated palliatively with chemotherapy or
radiation treatments and still be in hospice.
NICOLE FREEBOURN: And if you feel you want to come off hospice care, we can
discharge you. We’ll take you off and you can always come back on.
SELENA BOYETTE: The scope of hospice nursing in homes is kind of like Army
medicine, our team comes together and works really hard with what they have. Each
team is as individual as the people who are on them. And everybody brings their talents;
I have a nurse who takes her guitar because she knows a patient needs that.
DR. KAREN REICHOW: I tell my team at the hospital that everybody has to do the
work of the dying and sometimes you finish your work before you go and sometimes
you don’t, and it’s the people that don’t finish their work that have a little more difficult
time at the end of life. The work of the dying is to basically do five things: You have to
say forgive me, I forgive you, thank you, I love you, and goodbye. Some people don’t get
past the forgive me or they can’t even get there. So you have doctors, nurses, aids, the
chaplains, social workers, volunteers — one big team.
SELENA BOYETTE: Hospice is a Medicare benefit and we’re more and more
regulated, so there is more and more computer work and paperwork, but I think that
what keeps us coming back are those times we stop and sing at the bedside.
at the table
NICOLE FREEBOURN
education and
counseling to patients
and families. She has
worked at the VA
Medical Center and
Emory University
Hospital in Atlanta,
Georgia. Ms. Freebourn
holds a master’s
degree in social work
from the University
of Georgia.
at the table
BRETT BLIZZARD
Brett Blizzard is
a Wilmington
businessman, and
owner of Lumina
Lighting. He was
a caregiver for his
mother Evelyn
Blizzard at the
Davis Center and
the LCFH&LCC.
www.wrightsvillebeachmagazine.com WBM