Unmasking Suicide
BY Pat Bradford
WBM’s signature series returns with an in-depth roundtable discussion of how suicide has touched our community. Representatives from the medical education and pastoral fields and men and women who have lost loved ones to suicide gathered over a catered brunch with the goal of opening eyes to a rarely talked about evil plundering our county state and nation.
Date
Friday Sept. 15 2017
Location
The Airlie Road home of Haywood Newkirk
Brunch by Caterers
Brent Williams Brent’s Bistro and Dockside Restaurant
Court reporter
Tina Stancill
Flowers
Chelsea Fritts Fiore Fine Flowers
Table top and additional style
Estelle Baker Fisherman’s Wife
Chairs and bar stools
On loan from Cruz restaurant
Hair and makeup
EL Morea and Madeleine Hinton Bangz Salon
At the table:
William Scott Bennett Ph.D. clinical psychologist in private practice for more than 20 years. Private practice work includes treatment of anxiety and depression trauma recovery suicide prevention and various adjustment disorders.
Pat Bradford publisher editor and writer lost her brother publisher Tim Bradford in January 1997 to suicide.
Candice Noelle Brenneman outpatient therapist/owner Systemic Medications and Restorative Therapy and military family life counselor Fayetteville North Carolina. Works with the military military dependents and the public.
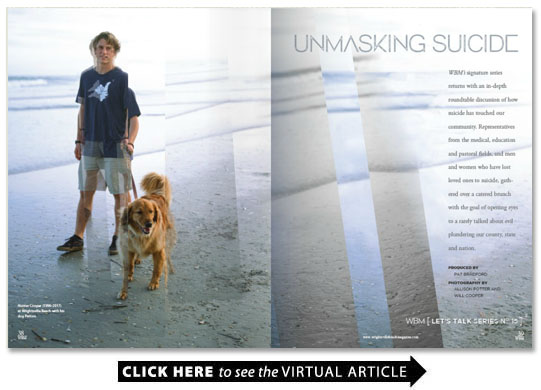
Alan W. Brown MD began medical career as a family physician went on to specialize in eye surgery. Was a contemporary and friend of Dr. Byron Stratos who took his life February 2010. His son Dillon and Hunter Cooper were best friends.
Jim Cooper businessman lost his wife Kim to suicide 9 years ago and his 21-year-old son Hunter in March 2017. Jim has been involved with Wilmington’s Touched By Suicide group as co-leader.
Gracelyn Elmendorf lost her husband of 21 years Skipper Duffee and her 19-year-old son Robert to suicide. Gracelyn founded Robert’s Hope in Florence South Carolina to educate students from grades 6-12 on depression suicide awareness and prevention. As an RN she has served as chair of the Mental Health America chapter in Florence.
Louise Rippy Lane lost her father Fred president of Rippy automotive. Co-leads Wilmington’s Touched by Suicide is on leave of absence from the North Carolina chapter of the American Foundation for Suicide Prevention.
Cristen Roggemann MEd. LCSW LCASA Therapist School Based Services Program Director Coastal Horizons Wilmington Health Access for Teens Clinic.
Rev. Adrian Shepard retired pastor lost his second of four sons Kirby age 16 in 1985 while living in Charlotte where he and his wife Joyce joined Touched By Suicide. Two years later they moved to Wilmington to serve as pastor of United Advent Christian Church. They helped organize Touched by Suicide in Wilmington. Their youngest son Kenny 36 died in January 2012 from a vicious infection.
Yuna Shin Cape Fear Community College German instructor and faculty advisor for the CFCC Feminist Alliance student organization. Hunter Cooper was her student.
MS. BRADFORD: I lost my brother Tim 20years ago. I’ve made it my goal to keep suicide from going laterally in my family. To bring awareness of how much risk your family is in once this has touched your family in any way.
DR. BROWN: Awareness is huge. I’ve been impacted by four different episodes. You’re watching this life and it’s like listening to a beautiful piece of music and then somebody suddenly lifts up the needle and they’re gone. The music has stopped and there’s a lot of confusion.
MS. BRADFORD: There were over 40 deaths by suicide in this county in 2014 and that’s higher than the number of people who died from breast cancer higher than the number of people who died from colon cancer. We’ve got to unmask this so it gets more publicity.
MS. Elmendorf: I believe the No. 1 myth is that if we talk about it it will suggest it to someone. It doesn’t. That’s all the more reason to be authentic and take our masks off and be vulnerable because people value vulnerability.
MS. ROGGEMAN: It’s not in socio-economic classes or races it really affects us all — it goes back to that adage it takes a village; it takes a whole community to really address the issue.
DR. Bennett: These things are also trans-generational. Somebody [died] who I was close to and they haven’t gotten over it or gotten through it they never processed it with anybody.
MS. BRADFORD: In my family to this day I cannot casually say ‘remember that time Uncle Tim did … whatever.’ They still can’t handle the conversation.
DR. Bennett: It keeps the pain intact. I tell my patients don’t waste your pain let’s deal with it let’s face it.
MS. Elmendorf: I lost my husband [to suicide] his grandfather took his life and then I lost my 19-year-old son in 2003. I started this presentation with young people in high school and I have found that the more isolated they are the more vulnerable they become. My son was a meek shy bullied Christian kid. Christian kids are really hard on themselves because if they blow it they think well it’s over I’m better off dead than alive.
Ms. ROGGEMAN: In our schools there has been a huge push for antibullying campaigns especially with the way people are interacting with social media.
DR. BROWN: Suicide is the ultimate bully. Maybe if we personified suicide and see it as not part of the person but a separate thing that’s bullying that person it might be a little bit easier to discuss it.
MS. BRADFORD: That actually is what it is isn’t it Alan?
DR. BROWN: It’s the ultimate bully.
MS. Elmendorf: We’ve got to educate people how to approach those who are considering suicide. Kids adolescents they are so much more able to cover up how they feel and they tell their friends not their parents. Teachers are on the front lines because they spend more time with kids than their moms and dads.
MS. SHIN: I was one of Hunter Cooper’s teachers at Cape Fear Community College. Everybody loved him and it was a real shock [when he took his life]. Afterwards it’s always in the back of my head ‘Could I have done something should I have seen something?’ Every one of the teachers at Cape Fear was left wondering what could we have done. My department chair and I are trying to figure out if there is something that we can do to help students with suicidal thoughts or depression.
MS. Elmendorf: I was mental health association chairperson in my community for threeyears. The Gatekeepers Training Class teaches what to look for how to approach kids. It’s called QPR; its emotional CPR. It stands for question your student persuade them to get help and then respond by taking them to get help. If you just comfort people by letting them know it’s OK you can’t do it wrong.
DR. Bennett: There’s something tremendously healing about emotional validation. When a person feels ‘Hey I’m not alone somebody gets me ‘ you’ve got your foot in the door. And I think most people will respond well to that.
MS. Elmendorf: They just want somebody to listen.
MS. BRADFORD: How do you emotionally validate someone?
DR. Bennett: They will express an emotion or you can deduce what their emotion is and you repeat it back to them. “I can tell that you’re really upset and bothered by this sounds like you’re feeling crushed.” They may have totally illogical reasoning for their depression or for how they feel. It doesn’t matter. What matters is that somebody has made that connection.
MS. ROGGEMAN: Something our community does is mental health first aid. It’s for people who are not trained but who are just interacting with others daily. It teaches people the signs to look for. Not everyone will say “I’m having a hard time and I want to end my life.” So what are the things that we need to pay attention to? And if we get it wrong then they are no worse off for getting the extra support.
MS. SHIN: As a result of Hunter I’ve been more sensitive to really looking at my students and seeing this person seems a little more tired today or they have dark circles under their eyes.
MS. Elmendorf: There is I believe a window of time usually about a week or so where they give you some clues because they’re asking for help. They don’t want to die; they just want to escape the pain.
MR. COOPER: After [my son] Hunter took his life in an article in the “Lumina News” I alluded to the fact that Hunter was taking a flu medication. A lot of people told me that they became suicidal after taking [a powerful well-known flu medication].
DR. BROWN: Hunter was best friends with my son Dillon. Everything was going well in Hunter’s life. When Jim told me he had recently been on a medicine for the flu as a physician that was a flag. There are so many side effects. [It] has been banned in Japan because they had so many young people taking their lives usually within the first two to threedays of taking the medicine. There should be awareness that it’s not a perfect medicine. Physicians need to be talking to patients if they prescribe it.
MS. Elmendorf: My son was very shy and awkward. He had seen a commercial about [a popular antidepressant] and he insisted on taking [it] and in sixweeks he was gone.
DR. Bennett: They are given just way too freely if not frivolously. Spikes in suicide often occur when a person begins or changes their medication.
DR. BROWN: Patients need to be really counseled: ‘We’re changing this medicine but here are some things I want you to look for ‘ and they need to talk to the family about that too. Byron Stratos was a colleague of mine an excellent eye surgeon and it’s my understanding that during a switch from one antidepressant to another is when he ended up taking his life.
MR. COOPER: There needs to be severe warnings about a lot of these medicines and how dangerous and powerful they are.
DR. Bennett: We should all be more skeptical about what is being thrown at us on TV and in magazines. We should be more inquisitive to our physicians about what is this going to do what are the side effects?
MS. BRENNERMAN: That’s true. I see a lot of veterans I have one who tried to take his life because no one was managing his medications. It was years of not sleeping and not being on the right stuff. He said “I wish I would have just taken a time out to really have someone listen to me about my medications. I had to be hospitalized to get people to listen to me.”
MR. COOPER: Hunter left a note and one thing that has haunted me he said “I don’t know why I’m doing this.” And that’s made me really think that it was the medication. It’s almost like it’s the push over the cliff. A lot of people have good results with anti-depressants and I’m not against them. I’m against the misuse and overreliance on medication.
MS. SHIN: It’s also very important to bring awareness to the fact that mental health is a health issue. We need health insurance to cover mental health.
DR. Bennett: The mental health profession has fallen short on advertising the benefits; we only talk about it when things go bad you need to come see one of us. But if we were bold and talked about how it helps I think we might make more inroads.
MS. BRADFORD: The words “mental health” are so stigmatized.
MS. Elmendorf: It’s a stigma. If you have an eye problem you go to the eye doctor. It’s your brain. Why is that so different?
DR. BROWN: You should call it brain health. I wonder if part of our normal physical exams kid’s sports exams if that should be a normal question: “Have you had any thoughts about hurting yourself?” Why not ask about brain health issues?
Ms. ROGGEMAN: On high school campuses in New Hanover County we have wellness centers and they really focus on integrated therapies. Kids get their immunizations they can get their sports physicals and there’s a mental health professional there. They can talk with somebody. I’m really trying to promote it as a wellness issue; you don’t just go when you’re sick. If you are doing well then keep coming and we’ll keep you well.
DR. BROWN: To avoid some of the stigmas we could just look at that like a car inspection. You say “How is your brain working have you had any problems with these type of thoughts or those type of thoughts?”
MS. Elmendorf: Another myth is ‘They were so selfish.’ It is not a selfish act at all. It’s a decision they make under this false belief that everybody will be better off without them. If there is onething that sums up anyone who takes their life it’s shame and disappointment.
DR. Bennett: Social media is proving to be a larger and larger component to making suicide an option. The irony is that you have the technology to reach everybody on the planet and yet we’ve never felt more disconnected. That has proven to be one of the largest variables in making somebody at risk for suicide. Another is perfectionism. When a person gets stuck into they have to be perfect or near-perfect (and of course who is) then they don’t know what to do with that. The hopelessness kicks in and then it’s a slippery slope.
Ms. ROGGEMAN: According to the CDC for our area the 24-to-34 age range has the highest completion rate [attempt vs. completion].
MS. Elmendorf: In the U.S. men are three times more likely to accomplish suicide than women.
MS. SHIN: I remember reading that women before they attempt to do it also advertise in a way that people pick it up. Men do not.
DR. Bennett: Men advertise it differently. They tend to be angrier; they tend to have more erratic behavior.
MS. BRENNERMAN: Women also are more likely to talk with someone. Men don’t really do that.
MR. COOPER: A lot of times the men manage the finances and they get in trouble and they’re ashamed to admit a failure. Or their business gets away from them and they see with a sick mind ‘My way to solve this for my family is to take my life and they’ll get the insurance and it can bail them out.’ A high percentage of men allow their jobs and their financial situation to define who they are. And it’s a lie.
MS. BRADFORD My brother had a complicated set of perceived failures.
MS. Elmendorf: That was the story with my husband. He felt like he was worth more dead than alive. He did what I call the farewell tour. He went to see all of his family members and wrote a very long letter to me with instructions on how to handle the finances and what to tell the children. I had been married to this man for 21years and I never saw it. But he did not mean for me to see it he hid it from me. It wasn’t just the business failure. The glass of water doesn’t overflow with the last drop it’s every consecutive drop that fills that glass and made that glass overflow. The last critical factor was losing the company. That made him feel so unworthy.
MS. BRADFORD: And hopeless.
MS. LANE: My dad took his life on a Monday. He had written in his planner to take Louise to lunch next week; take Louise and husband and Mom to dinner the next weekend. So it was kind of planning double lives. Like if I wake up tomorrow and I feel better then you know we’re going.
MS. BRADFORD: My brother his was all planned out. He visited with his friends. Can you imagine what they felt like that they didn’t see? The guilt just splattered. It was almost like a concentric rain out into the community. The stigma was so deep that at the funeral they pretended like it hadn’t happened almost like he’d been in a car accident or something.
MS. Elmendorf: It doesn’t have to be a dysfunctional family. We can be a happy family but sometimes the mental health issues are there.
MS. SHIN: Has there been a study in mapping out the genetics of depression so you would know if you are at risk or not? Obviously if there has been a suicide in the family you are at risk.
MS. BRADFORD: Absolutely. When my brother took his life my husband took a job where he was gone for three weeks at a time. So there I was alone in my grief. Just because you’re a Christian doesn’t mean you’re not at risk. Working I had the mask on all day long but at night it was really dark. And it got to the point where I was hopeless and wanted to stop the pain. I believe I felt what my brother felt when he couldn’t go on any longer that exact point –feeling I was trapped there was no way out. I did ask for help and I came back from that place. But I’m concerned about the people in my family that are holding onto the anger.
DR. Bennett: It’s easier to get through the day with denial. Not through the week or the month or the year but through the day. Denial can be deadly.
MS. BRADFORD: The family member that’s grieving over the loss of a family member they’re in denial of what?
DR. Bennett: Denying the grief.
MR. COOPER: Or they won’t talk about it. They won’t engage or even mention it.
MS. Elmendorf: Sometimes they don’t want to talk about suicide in that immediate family group because they are dealing with their own concerns of could have would have should have. Then sometimes they are blaming someone else in the family and it’s easier just to keep it quiet than to deal with it.
MR. Shepard: I lost a son in 1985 16 years old and one of the things that became really obvious to us this whole idea of how men have that exterior of strength and resourcefulness. He and his best friend were both in love with the same girl and he saw himself losing so he took his life. Here was a kid who looked strong seemed strong exterior was intact in most ways but deep down he was hurting.
MS. Elmendorf: Probably the number one reason young people take their lives is the significant loss of a loved one whether it’s a boyfriend or girlfriend or a parent. They don’t understand that things can get better tomorrow. They don’t understand that the school they don’t get into or that girlfriend that turned her back on them that can get better tomorrow.
MR. Shepard: I believe my son if he could have had a next week he probably still would be here. We were in Charlotte. A small group started there Touched by Suicide where I felt I could share I could open up. And then some families wanted to do something like that here. I could lead the groups help people to share with each other but I could also go back home and draw into my shell and be that person that didn’t pay as much attention to family friends or people with needs.
MR. COOPER: My wife died in 2008. She became clinically depressed. She ended up taking her life. I call it ending her pain. I got involved with Touched by Suicide and I started seeing so many people that once someone in their family took their lives they became stuck. It was like swallowing something and it wouldn’t go any further. It was almost like they were trapped.
MS. Elmendorf: I do know one thing: If love could keep these people alive I would still have a husband you would still have a wife and son I would still have a son. Ultimately it is their decision and we can do everything right and they can still make that decision.
MR. COOPER: I really asked God for a strategy how to help people move forward and not allow that event to define their lives. I really believe with all my heart you can still have happiness and joy and you can have a wholesome life.
MS. Elmendorf: [The group setting] gives you a chance to tell your story because you need to tell your story over and over again. I see it like a kaleidoscope every time you tell it you give it a little turn and it sort of rearranges things so you can kind of separate the fantasy part of it. You heal a little bit every time when you give it a voice.
MR. COOPER: Some people really like the fact that everybody [there] gets it. I can actually talk about it because all of you really understand you know how I feel and my friends don’t so I don’t talk about it.
MR. Shepard: Our group has had to discuss how does a mother communicate to younger children the loss of a husband or a father?
MS. LANE: The best thing is to tell them in a way they can understand it. Nicole Ward [Byron’s widow] had kids ranging from 5 to 15. She explained it to the youngest ones — like think about a heart attack — your dad had a brain attack.
DR. Bennett: Parents are quick to say oh I’m going to protect my child and really what they’re doing is protecting themselves from having that conversation. But if you don’t talk about it the unintended message is well you can’t handle it. You want to give them a chance to handle it and help them handle it and find out whether they are handling it.
MS. BRADFORD: We need to get the word out to ask the “how” question. I could ask “How are you doing emotionally today Jim ” but I’ve been a little scared to ask you. We need to ask people the healthy people the people who maybe are sitting in the back of the classroom. Sometimes the kid that’s the brightest or the quickest to raise their hand is the one that maybe has something they’re hiding. It’s different for every person but we can be asking them how are you feeling today what’s going on in your head today?
DR. BROWN: How is your brain working?
MS. BRENNERMAN: Just checking in with people and that it’s okay. A lot of them don’t have anyone that checks in for them so that’s huge.
MS. BRADFORD: If I was speaking in front of 1 000 people and I said “This happened to me how many people have thought about taking their own life or have been touched by suicide?” About 98 percent would raise their hands. If we all just say “Hey I read this article on suicide … how is your head working ” maybe we can get a conversation started.
Ms. ROGGEMAN: It’s more than just asking the question. It’s really listening to verbal and nonverbal answers.
DR. Bennett: So you say good? Define good? What’s good? What’s not so good? Probe a little bit.
MS. Elmendorf: We have to think about who they were while they were here because we so focus on the negative things and the pain. There’s an article by Norman Vincent Peale that I love about a sermon he had heard. It gives a whole different perspective to suicide. It talks about let’s give this person credit for all of the silent battles that he fought and did win before he took his life. Let’s remember who he was and not let this one final act define who he was because we don’t know the silent skirmishes this person fought for years to maintain who he was for as long as he did.
MS. SHIN: Hunter sent me an email on [that] Wednesday he said I’m sick I won’t be in class today I will see you on Friday. And then Hunter took his life on Thursday. So I went back to the email and I said do I see anything here? And I said no I don’t see anything. I couldn’t have because he was happy and he said he would see me on Friday. I mean who does that?
MS. BRADFORD: Every one of us had that same guilt. We all asked “What could I have done different? How come I didn’t see this? What did I miss?” It’s part of the evil trying to get you too. Don’t think that don’t go there.
MS. Elmendorf: It’s important as a believer to turn that why question into ‘What purpose do I suffer Lord?’ because I think He can use your suffering.
MR. COOPER: The why question is a dead-end road. But for what purpose do I suffer? God can you possibly use this for good in our lives to help other people? That is a life-giving highway.
MS. BRADFORD: Romans 8:28 and 29 say that the Lord will turn a bad thing for good. Nothing bad is EVER His doing — but He does take a bad thing and turn it for good. In my case I’m mentally healthy. In Hunter’s case it’s drawing young people together and hopefully the awareness will really spread in that generation. Your annual Out of Darkness Walk is a great way to get public awareness out.
MS. Elmendorf: The more we talk about it the more we get it out there the less stigmatizing it will be the more we are giving pain and depression a voice and a face of normalcy. And I love what the pastor said at Jim’s son Hunter’s funeral: “It’s OK not to be OK.”
“Communities play a critical role in suicide prevention. They can provide social support to vulnerable individuals and engage in follow-up care fight stigma and support those bereaved by suicide.” — World Health Organization 2014
Risk Factors For Suicide
It is estimated that between 6 and 32 survivors exist for each suicide.
A survivor is a family member or friend of a person who has died by suicide.
Surviving the loss of a loved one to suicide is a risk factor for suicide.
Surviving family members and close friends are deeply impacted by each suicide and experience a range of complex grief reactions including guilt anger abandonment denial helplessness and shock.
Source: National Suicide Prevention Lifeline
In the United States
Suicide is the 10th leading cause of death. Each year 44 193 Americans die by suicide.
There are an average of 121 suicides per day.
In 2015 the highest suicide rate (19.6 per 100 000) was among adults between 45 and 63. Adolescents and young adults aged 15 to 24 had a rate of 12.5 per 100 000.
Men die by suicide 3.5 times more than women.
Firearms account for 49.8 percent of all suicides.
White men accounted for 7 of 10 suicides in 2015.
There are 24 attempts for every completed suicide.
Suicide costs society over $51.9 billion a year.
Source: The American Foundation for Suicide Prevention
Preventing Suicide: A Global Imperative
Everyone plays a positive role in suicide prevention. Communities peers close individuals and the media are critical in preventing death by suicide. If you are concerned about a friend or loved one:
Be direct. Talk openly and matter-of-factly about suicide.
Be willing to listen. Allow expressions of feelings. Accept the feelings.
Be non-judgmental. Don’t debate whether suicide is right or wrong or whether feelings are good or bad. Don’t lecture about the value of life.
Get involved. Become available. Show interest and support.
Don’t dare him/her to do it.
Don’t act shocked. This will put distance between you.
Don’t be sworn to secrecy. Seek help.
Offer hope that alternatives are available but do not offer general reassurances such as “it will get better” or “it could be worse.”
Get help from persons or agencies specializing in crisis intervention and suicide prevention such as Military Crisis Line.
�– United States Department of Defense
12 500 people participated in the Out of Darkness Walk for Suicide Prevention at Wrightsville Beach last November.
North Carolina Suicide Fatalities 2015
Statewide 1 406 (Death Rate per 100 000 residents: 14)
New Hanover County 26 (Death Rate per 100 000 residents: 13.2)
Brunswick County 17 (Death Rate per 100 000 residents: 13.8)
Pender County 10 (Death Rate per 100 000 residents: 17.4)
Onslow County (home to Camp Lejeune) 52(Death Rate per 100 000 residents: 16.1)
Cumberland County (home to Fort Bragg) 34 (Death Rate per 100 000 residents: 18.2)
Source: North Carolina State Center for Health Statistics
Military stats on Suicide
In 2013 the Unites States Department of Veterans Affairs released a study that covered suicides from 1999 to 2010 which showed that roughly 22 veterans were dying by suicide per day or one every 65 minutes. Some sources suggest that this rate may be undercounting suicides.