Wearable MedTech Advances
Sensor-equipped clothing, patches and devices
BY Joe Jancsurak
Fitbits and smart watches are just the beginning when it comes to wearable devices for a healthier you. By the end of the decade, advanced sensor-equipped garments, patches, and wearable microneedle technology could improve quality of life for individuals with chronic conditions such as Parkinson’s and heart conditions while providing early indicators for infectious diseases including COVID-19.
Wearable continuous glucose monitoring (CGM) systems are already in use. These devices measure levels beneath the skin without finger sticks through wearable sensors coupled with handheld transmitters. The transmitters send glucose numbers to a smart phone or display device.
The latest offering, approved in Europe but not yet in the United States, combines the sensor and transmitter into one device, making for a small square-shaped offering positioned on the back of the upper arm.
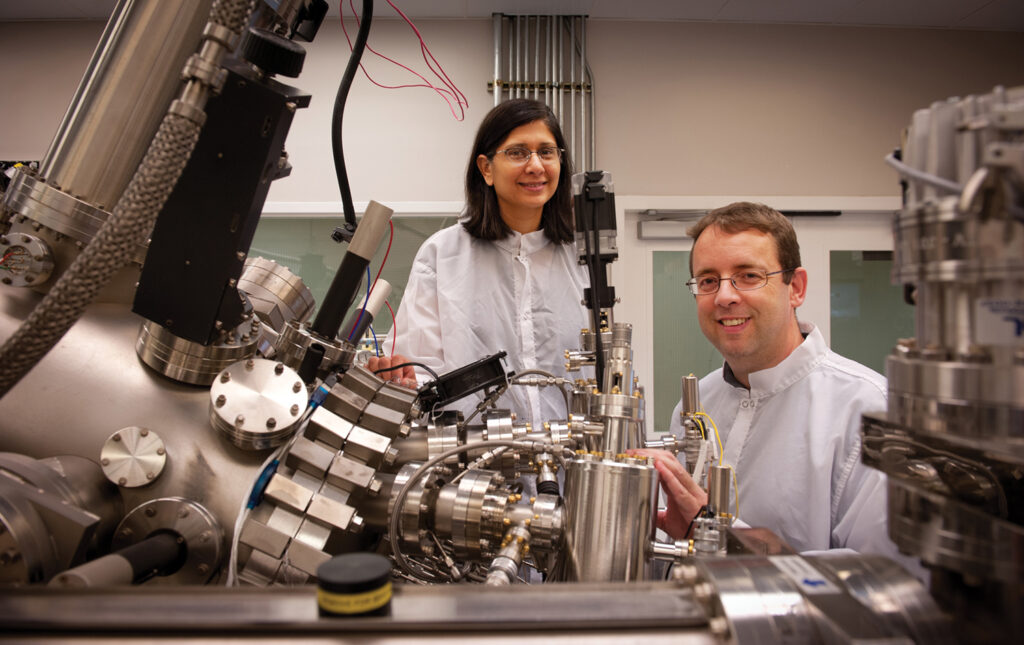
Research scientists nationwide, including in North Carolina, are working on breakthrough wearable and implantable innovations, including “smart” clothing.

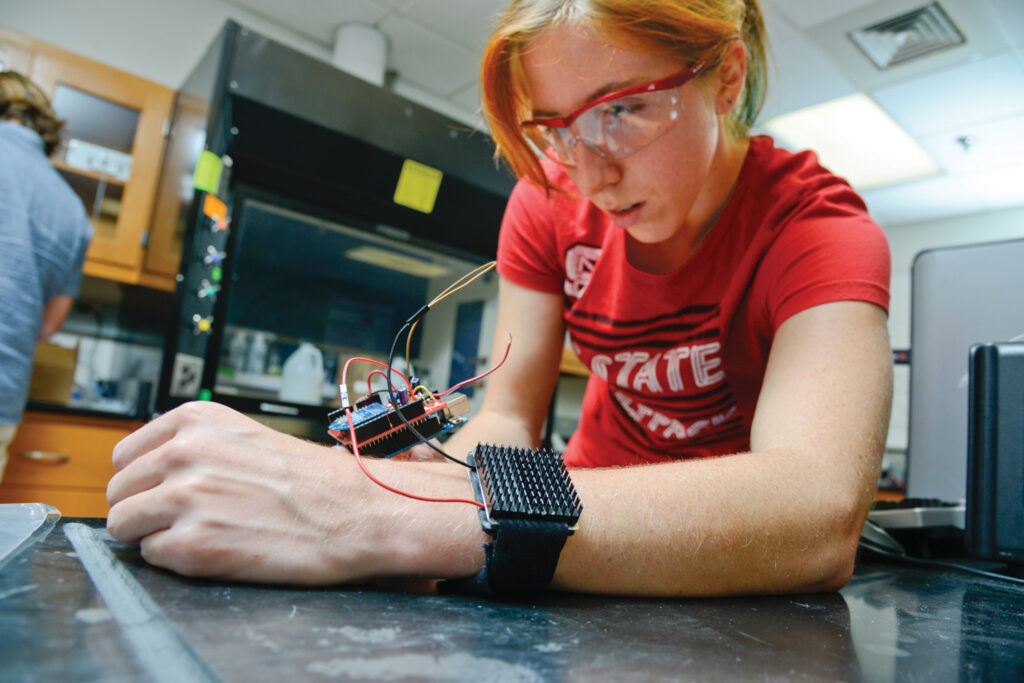
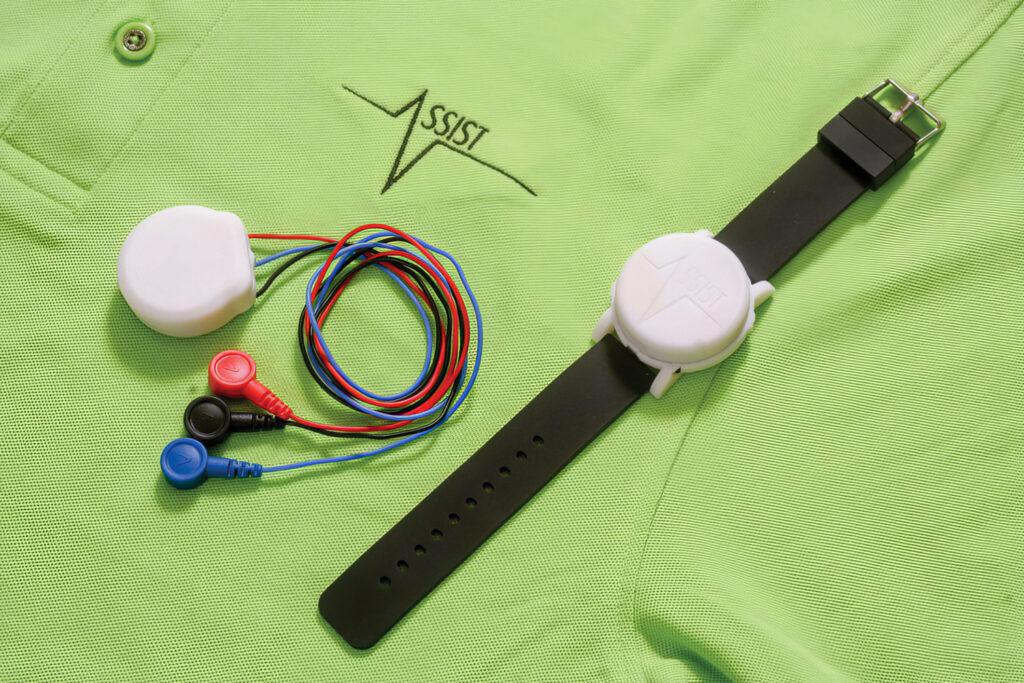
That’s one of the many developments being spearheaded by ASSIST, an acronym for the Center for Advanced Self-Powered Systems of Integrated Sensors and Technologies. Started in 2012, the initiative is a seven-university research and development program led by NC State in Raleigh, where Ravi Chilukuri manages an innovation ecosystem composed of faculty, industry and government representatives, and the medical community.
“While still in the early stages of R&D, we are working with industry partners to bring together flexible electronics and textiles to develop various self-powered wearables and smart fabrics, including smart watches, rings, armbands, shirts, pants and sports bras to track various physiological and biochemical markers such as blood oxygen, glucose and lactate levels, uric acid, body temperature, heart rates, and to provide ECG (electrocardiograph) and EMG (electromyography) readings,” says Chilukuri. “Such devices could be worn by patients with chronic conditions, including diabetes, dementia and heart disease as well as detecting cough, speech or gait and monitoring wounds, sleep or stress.”


The challenge is getting the devices powered by the body’s motion and thermal radiation so they would never need recharging.
“The diagnostic information would be gathered and communicated through a smart phone device to provide users with data for predictive analytics that would be used for providing recommendations,” Chilukuri says. “The data could also be tracked by physicians practicing telemedicine.”
Huanyu Cheng, associate professor of engineering science and mechanics at Penn State University, is working on similar technology.
“It is possible to design circuits with different modalities that not only monitor blood pressure and heart rates, but also recognize and track inflammatory biomarkers,” Cheng says.
Inflammatory biomarkers can be early indicators of infections such COVID-19, thyroid conditions, cancer, and autoimmune disorders such as lupus, rheumatoid arthritis and inflammatory bowel disease.
“Our research group is developing nanosensor-equipped microelectronic systems that can be incorporated to medical-grade silicone patches worn by the patient,” Cheng says.
Just how small are these nanosensors? They are one-billionth of a meter. For the sake of comparison, a sheet of paper is about 100,000 nanometers thick. The systems, which are under development and awaiting adoption by a large medical device company, feature a foam layer with embedded electronics. They are applied to the skin with an adhesive, much like a removable but “robust tattoo,” says Cheng.
“The electronics are complex, and the biocompatible materials must work in harmony with natural skin motion,” he says.
Also under development by Cheng’s team are biodegradable implantables made of “essential metals” such as zinc and magnesium and dissolvable substrates made of silk, silicon and even rice paper. Implantable cardiac monitors currently are widely used, but battery life is limited and require them to be surgically removed after about three years.
Cheng says wearable patches could be prescribed by physicians within the next year. The wait for the implantables will be longer due to a more rigorous Food and Drug Administration approval process.
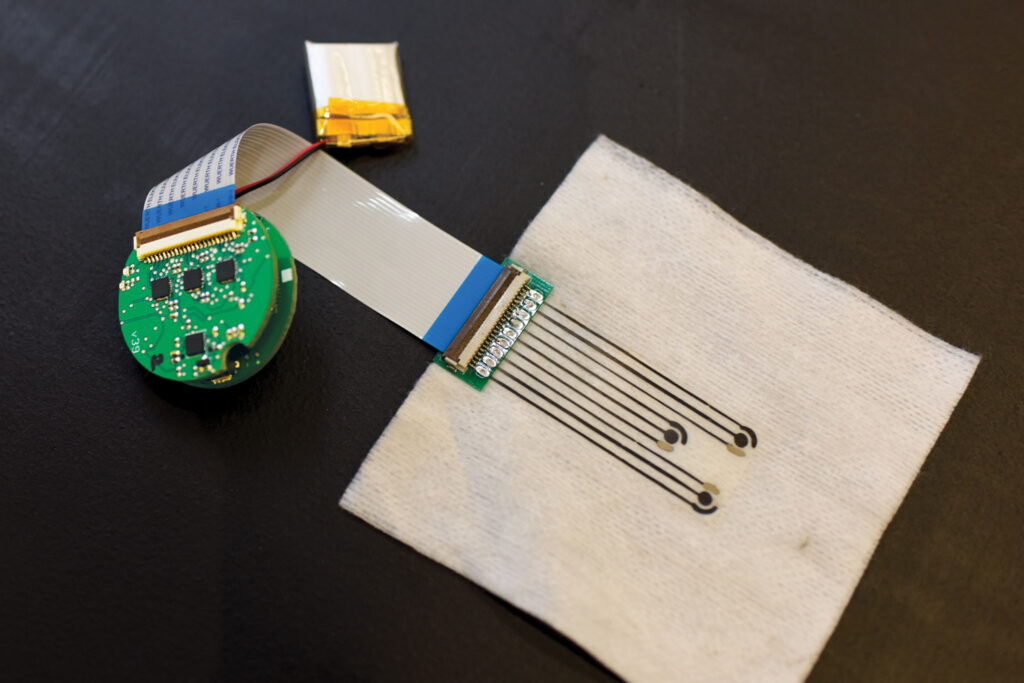
At Sandia National Laboratories, a federal research and development organization in Albuquerque, New Mexico, device development includes microneedles the size of a micron, or one millionth of a meter. That’s roughly one-tenth the thickness of plastic cling wrap. The tiny needles are currently used in micron-scaled patches for transdermal drug delivery applications to treat chronic pain, chemotherapy-induced nausea, attention-deficit/hyperactive disorder (ADHD), and smoking cessation.
“Now we are developing transdermal microneedle-equipped monitors for painlessly accessing interstitial fluid in the skin to monitor biomarkers that include cytokines, small proteins that when found in small amounts can help control inflammation, allowing the immune system to protect against illness,” says Ronen Polsky, materials scientist at Sandia. “Rising cytokine levels, which may cause inflammation, may occur in response to certain treatments such as immunotherapy, leading to sepsis, metabolic disorders, and cancer. Earlier access to this data could change and save lives.”
Ram Mishra, a senior research scientist at BioSensics, a company in Newton, Massachusetts, specializing in wearable sensors and digital platforms, says wearables can serve as valuable tools for empowering patients to participate in their health management, reducing the caregiving burden.
For example, wearables with accelerometers and advanced algorithms can be used for monitoring remote and prolonged physical activity, including sit-to-stand transitions associated with lower leg muscle mass, which often undergo atrophy with aging or a sedentary lifestyle, or the number of steps taken during daily walks.
Similarly, sensors with gyroscopes can be utilized to evaluate balance deterioration resulting from impaired postural control, commonly associated with neurodegenerative diseases. This information can be beneficial during medical appointments or for adjusting a care plan. If a wearable indicates a decline in activity levels, care-plan modifications can be implemented to encourage increased physical activity. Or, in the event of a fall, the device can automatically alert caregivers or emergency services.
Additionally, in a sensor-equipped home, the rooms and spaces where the patient is most active can be monitored.
BioSensics recently introduced a smart home technology known as iADLSYS, which has the capability to identify interactions between the person wearing a pendant sensor and various objects within the home tagged with pTAG sensors. This technology could provide an objective measure for assessing the risk of urinary infections based on the frequency of bathroom usage. Monitoring the use of a medicine box could assist in determining a patient’s adherence to medication regimens. Currently, gaining such information can be challenging when dealing with dementia patients.
As for the future of wearable medical devices, Polsky says, “Look for artificial intelligence to play an important role in propelling predictive medicine.”
Smart devices could be used to diagnose conditions that if left untreated could cause or advance illness, thereby enabling either prevention or early treatment of a disease.
Another possibility would blend the upcoming data analytics-driven diagnostics technologies with therapeutics.
“For example, wearables would not only show high sugar levels, but they could also provide insulin on a per-need basis,” says Chilukuri.
Or the devices could blend diagnostics with haptics (using touch and tactile feedback) for applications in rehabilitation and physical therapy.
FDA approvals and the support of insurance companies will be required for such advancements to take hold.
“Insurers need to support wearables for patients so physicians can prescribe the devices,” Mishra says. “Everyone gains, including the insurance companies, when a medical condition is improved, or better yet, prevented.”
ASSIST program’s annual challenge for Middle and High School students
Every year teams of high school and middle school students participate in an annual wearable device for humans and animals challenge at NC State College of Engineering. In its ninth year, the competition is put on by the Center for Advanced Self-Powered Systems of Integrated Sensors and Technologies (ASSIST) led by NC State. ASSIST began as a National Science Foundation Engineering Research Center in 2012. This year’s competition will be held on April 16, 2024.

